Chronic pain, anxiety, and depression share many things in common. They are all serious health conditions that can have a detrimental impact on a person’s quality of life. They affect both the mind and the body, and they often occur simultaneously or as a result of each other. Not surprisingly, these conditions can be addressed together by treatments with multifaceted benefits for mental and physical wellness. In this article, we explore the connection between these conditions and unpack specific treatment methods that can target all three.
How Are Chronic Pain, Anxiety, and Depression Related?
For many people, chronic pain, anxiety, and depression are interconnected. Dealing with chronic pain can be mentally taxing and lead to the development of depression and anxiety. On the other hand, severe anxiety and depression can feel physically painful. For example, anxiety can manifest itself in the form of sharp chest pain or constant muscle tension. All three conditions can have a negative impact on mental and physical health, resulting in decreased sex drive, weight fluctuations, fatigue, sleep disturbances, and decreased self-esteem.
Conditions That Cause Chronic Pain and Co-Occur With Anxiety and Depression
Here are some common conditions that cause chronic pain and have a connection to anxiety and depression:
Arthritis
Arthritis is a joint condition where one or more of your joints experience swelling and tenderness. It can lead to limited mobility and chronic pain. The three most common types of arthritis are psoriatic arthritis, osteoarthritis, and rheumatoid arthritis. Depression and anxiety can worsen arthritis by increasing pain perception. These mental illnesses can also cause muscle tension and inflammation, leading to increased joint discomfort.
Fibromyalgia
Fibromyalgia is a chronic condition that causes pain throughout the body. Symptoms include dull aches that last for months and cause muscle and joint stiffness. Those who suffer from fibromyalgia may find it painful to perform daily activities, such as walking or lifting heavy objects. When fibromyalgia is linked with mental health disorders, such as anxiety and depression, it can heighten the body’s pain response. Anxiety can lead to muscle tension and exacerbate pain and stiffness.
Multiple Sclerosis
Multiple sclerosis (MS) is a chronic autoimmune disease that affects your central nervous system. It damages the protective covering of your nerves and disrupts communication between your brain and body. This condition is sometimes associated with mood swings, anxiety, depression, and obsessive-compulsive disorder (OCD). Those who experience fibromyalgia and depression simultaneously may feel the urge to withdraw socially, making it more difficult to seek support and adhere to treatment plans.
Chronic Migraines
Migraine is a neurological condition characterized by frequent headaches that last from a couple of hours to a couple of days. Other symptoms include vomiting, light sensitivity, nausea, and blind spots. Over time, the emotional stress of migraine can lead to the development of depression and anxiety. In fact, people who suffer from migraine are about five times more likely to develop depression than those who do not suffer from it. On the other hand, depression can lead to frequent and severe headaches, meaning that mental illness can precede or follow the development of migraine. Over time, migraine and mental illness can significantly reduce your quality of life.
Treatment and Therapies
Dealing with chronic pain can be overwhelming, especially when it is accompanied by mental health problems like anxiety and depression. Several forms of treatment can help you improve your emotional and physical well-being simultaneously, including:
Cognitive Behavioral Therapy
In cognitive behavioral therapy, patients can talk with a therapist to navigate the emotional challenges associated with anxiety, depression, and chronic pain. This form of treatment can help you change your thought patterns and develop coping strategies for physical and emotional discomfort. It can also reduce feelings of isolation by making you feel heard and understood.
Massage
Massage can provide relief from physical and mental tension for people living with chronic pain, anxiety, and depression. It improves blood circulation, promotes relaxation, and can alleviate pain in specific areas, such as the neck, back, and shoulders. Massage therapists can tailor their techniques to your specific condition for the best results.
Transcutaneous Electrical Nerve Stimulation (TENS) Therapy
TENS therapy is a non-invasive treatment that uses low-voltage electrical currents to manage pain. It can provide instant relief from chronic pain and is often used with other treatments, including medication and physical therapy. Its pain-relieving effects can positively impact mental health and may help manage anxiety and depression resulting from chronic pain.
Double-Duty Medication
Certain types of antidepressants prescribed for anxiety and depression can also relieve chronic pain. They include tricyclic antidepressants (TCAs) and serotonin and norepinephrine reuptake inhibitors (SNRIs). However, these drugs are more effective at alleviating nerve pain than other types of pain. Before starting a course of treatment, you should consult a healthcare professional to determine whether antidepressants are the right option for you.
Physical Therapy
Physical therapy aims to improve mobility and reduce pain through strengthening exercises and stretches. It promotes blood circulation and healing. In addition, exercise has been scientifically proven to lessen symptoms of anxiety and depression. It can improve your mood and boost your self-esteem.
Acupuncture
Acupuncture addresses pain by improving energy flow (qi) in your body. It involves needles being inserted into specific points to release tension and promote relaxation. This form of treatment can be effective in treating chronic pain, anxiety, and depression when practiced regularly and combined with other types of therapy.
Community Support Groups
This form of therapy allows you to connect with people who understand your experience. It can provide you with a safe space to share your thoughts and receive emotional support. There are many support groups for anxiety, depression, and chronic pain. Joining a community support group can help you build resilience and confidence through the creation of meaningful connections and shared vulnerability.
Biopsychosocial Approach: How This Model Heals Physical and Mental Health Conditions
The biopsychosocial approach is a proven method to manage chronic pain and mental conditions associated with physical discomfort. This approach suggests that chronic pain does not develop in isolation. It actually manifests due to a variety of individual factors, including biological, psychological, and social factors. Doctors apply the biopsychosocial model of pain management to better understand a patient’s biological and medical history and the psychological factors that may be impacting their health, such as stress factors, behavior patterns, a history of anxiety and depression, coping strategies, and social factors, including socioeconomic background, family dynamics, and work life. This comprehensive model significantly supports the development of personalized treatment methods to address physical and mental health conditions.
Holistic Care
The biopsychosocial approach looks at all possible problems, beyond the bodily issues, that could contribute to chronic pain. These problems may be related to an individual’s psychological or social well-being. As a result, doctors can apply this model to create a comprehensive, holistic treatment plan that benefits patients in the long term.
Improved Treatment
Healthcare providers have been using the biopsychosocial model of pain management to create more comprehensive and personalized treatment plans. Since this model considers all possible factors underlying physical and mental conditions, it offers improved treatment methods with a higher likelihood of successful outcomes.
Better Patient Engagement
The biopsychosocial model gives patients assurance that all their possible problems, including biological, psychological, and social issues, are being addressed together in one place. As a result, patients are more likely to trust the recommended treatment methods and are to actively participate in treatment protocols.
Multidisciplinary Approach
The biopsychosocial model is a multidisciplinary approach that takes into account different biological, psychological, and social factors that may contribute to issues like chronic pain, depression, and anxiety. This comprehensive model involves a multidisciplinary treatment approach that may include physical therapy, counseling, medications, and other interventions, increasing the likelihood of successful treatment.
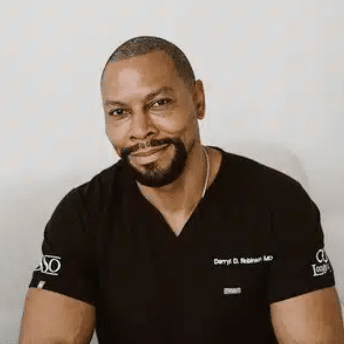
Oklahoma Spine and Pain Management Can Help
Chronic pain, anxiety, and depression are common problems for many patients. Previously, these problems were commonly evaluated and treated separately. However, modern advancements in medicine indicate that chronic pain, anxiety, and depression may not develop in isolation and are affected by a variety of biological, psychological, and social factors. At Oklahoma Spine and Pain Management, we utilize comprehensive, proven models, including the biopsychosocial model, to evaluate and treat chronic pain, anxiety, depression, and other conditions. Schedule an appointment today for a detailed evaluation.
Frequently Asked Questions (FAQs)
How does chronic pain affect mental health?
Chronic pain makes it difficult to perform everyday activities. It can impact your ability to focus, sleep, and interact normally with others. It can lead to feelings of hopelessness and contribute to the development of mental health issues like anxiety and depression.
How do antidepressants help chronic pain and depression?
Antidepressants address chronic pain and depression by altering your brain chemistry. They increase serotonin and noradrenaline levels in your brain, improving mood and blocking pain signals.
What is the biopsychosocial model in pain management?
The biopsychosocial model in pain management is a proven approach that suggests that chronic pain does not necessarily develop in isolation. It may be related to several factors in a patient’s life, including biological, psychological, and social factors.
How can a biopsychosocial approach improve treatment outcomes for chronic pain and depression?
A biopsychosocial approach takes into account biological, psychological, and social factors that may be contributing to chronic pain and depression. Identifying the relationships among these factors helps healthcare providers develop more personalized and effective treatment plans, improving treatment outcomes.
Is the biopsychosocial model used in clinical practice for chronic pain treatment?
Yes, the biopsychosocial model is widely and successfully used in clinical practice for chronic pain treatment. It’s a proven multidisciplinary approach that helps pain management specialists and therapists accurately diagnose an individual’s condition and recommend the most appropriate combination of treatment methods.